 Psychiatry Science Keeps Moving
Psychiatry Science Keeps Moving
Some recent readings I have come across…demonstrate that conceptual changes are always on the horizon. Two new areas of thinking about depression are emerging from basic and clinical research on brain inflammation and ketamine, an NMDA receptor antagonist. I’ll start with something old: attachment and mother love–a stunning video.
I first put up this BLOG post Dec. 11, 2012 and am revising it today because of new information about Ketamine and Treatment Resistant Depression. The video is charming and informative, so I am leaving the old post and adding the new information at the end.
To begin, a magnificent and chilling video on YouTube of “The Still Face Experiment” by Ed Tronick PhD. Illustrating the power, subtlety, and, wordlessly, the mechanism of mother-child bonding and attachment. Twenty-five years ago this too was revolutionary, now it is intuitively understood (in our culture).http://youtu.be/apzXGEbZht0
To my mind, the most revolutionary change on the horizon concerns brain inflammation and depression. We have to extrapolate from an article published online in September for the Archives of General Psychiatry , “A Randomized, Controlled Trial of the Tumor Necrosis Factor Antagonist Infliximab for Treatment-Resistant Depression” It is not surprising that it has taken a little time for the implications of this post to be taken up in the psychiatric community. Here are the basic points as abstracted in Psychiatric News[1], a publication of the American Psychiatric Association: The study showed that a biologic medication was able to reduce depressive symptoms in some subjects who had suffered from major depression for an average of 15 years. Specifically, an inhibitor of cytokine tumor necrosis factor reduced depression in subjects who had a high level of inflammation at the start of the study and had no effect on treatment-resistant patients who did not have high baseline levels of inflammatory markers. The drug involved, Infliximab, is a monoclonal antibody that is currently prohibitively expensive, $1,000 to $2,000 a month. But the science is encouraging.
The measure of inflammation was the common c-reactive protein. The infliximab subjects who had had a concentration of C-reactive protein greater than 5 mg/L at the start of the study experienced a significantly greater decrease in depression symptoms than the placebo group did. However, the placebo group experienced a significantly greater decrease in depression than did infliximab subjects with a baseline C-reactive protein concentration of 5 mg/L or less. Other drugs that have been used to manipulate the immune system in depression and other psychiatric diseases, include minocycline, aspirin, and COX-2 inhibitors—so it appears that a new paradigm is emerging.
 A different direction in biological psychiatry and depression comes from the numerous recent studies pointing to Ketamine’s rapid antidepressant effect. Ketamine has been considered a hallucinogenic club drug (it was responsible for John C Lily’s fixation on his conversations with alien beings), but it is currently used primarily as a pediatric (and animal) anesthetic because of its dissociative qualities. The first clinical study with depression was reported by R Berman in the journal Biological Psychiatry in 2000[2]: Replications of these effects with finer-grained explanations of the mechanisms of action have been coming in rapid succession lately. Jon Hamilton prepared a nice summary piece for NPR (available at http://www.npr.org/blogs/health/2012/10/04/162299564/ketamine-relieves-depression-by-restoring-brain-connections) in which he quotes one researcher, Ron Duman a psychiatarist and neurobiologist at Yale University, saying that this discovery “represents maybe one of the biggest findings in the field over the last 50 years.” Dunman is the lead author of a review in Science published Oct. 5, 2012.
A different direction in biological psychiatry and depression comes from the numerous recent studies pointing to Ketamine’s rapid antidepressant effect. Ketamine has been considered a hallucinogenic club drug (it was responsible for John C Lily’s fixation on his conversations with alien beings), but it is currently used primarily as a pediatric (and animal) anesthetic because of its dissociative qualities. The first clinical study with depression was reported by R Berman in the journal Biological Psychiatry in 2000[2]: Replications of these effects with finer-grained explanations of the mechanisms of action have been coming in rapid succession lately. Jon Hamilton prepared a nice summary piece for NPR (available at http://www.npr.org/blogs/health/2012/10/04/162299564/ketamine-relieves-depression-by-restoring-brain-connections) in which he quotes one researcher, Ron Duman a psychiatarist and neurobiologist at Yale University, saying that this discovery “represents maybe one of the biggest findings in the field over the last 50 years.” Dunman is the lead author of a review in Science published Oct. 5, 2012.
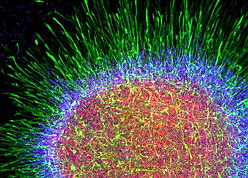
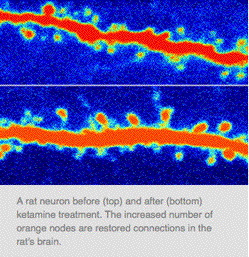 The abstract from Science follows: Basic and clinical studies demonstrate that depression is associated with reduced size of brain regions that regulate mood and cognition, including the prefrontal cortex and the hippocampus, and decreased neuronal synapses in these areas. Antidepressants can block or reverse these neuronal deficits, although typical antidepressants have limited efficacy and delayed response times of weeks to months. A notable recent discovery shows that ketamine, a N-methyl-d-aspartate receptor antagonist, produces rapid (within hours) antidepressant responses in patients who are resistant to typical antidepressants. Basic studies show that ketamine rapidly induces synaptogenesis and reverses the synaptic deficits caused by chronic stress. These findings highlight the central importance of homeostatic control of mood circuit connections and form the basis of a synaptogenic hypothesis of depression and treatment response.
The abstract from Science follows: Basic and clinical studies demonstrate that depression is associated with reduced size of brain regions that regulate mood and cognition, including the prefrontal cortex and the hippocampus, and decreased neuronal synapses in these areas. Antidepressants can block or reverse these neuronal deficits, although typical antidepressants have limited efficacy and delayed response times of weeks to months. A notable recent discovery shows that ketamine, a N-methyl-d-aspartate receptor antagonist, produces rapid (within hours) antidepressant responses in patients who are resistant to typical antidepressants. Basic studies show that ketamine rapidly induces synaptogenesis and reverses the synaptic deficits caused by chronic stress. These findings highlight the central importance of homeostatic control of mood circuit connections and form the basis of a synaptogenic hypothesis of depression and treatment response.
Interestingly, a week later Neil Fournier, also from Yale, presented parallel research at a Society of Neuroscience conference; the study, on rats, had implications that ketamine could be used to treat patients with post-traumatic stress disorder (PTSD). After conditioning rats to fear a particular tone, the researchers gave the animals ketamine or saline, then retrained them not to fear the tone. The next day, the rats that had been treated with ketamine were more likely to recall the new, positive association and less likely to exhibit fear-related freezing behavior when the tone was played, while saline-treated rats tended to recall the original, bad association. The findings suggest that a combination of exposure therapy and ketamine may help improve treatment for PTSD and other anxiety disorders.
Update: Since the original post on November 5, there have been many more ketamine-related stories. The most recent was a bulletin from the American Psychiatric Association this morning as follows.
In a genomewide association study of some 1,800 subjects, Japanese scientists have identified a gene on chromosome 2 that appears to influence both pain sensitivity and susceptibility to substance dependence. In fact, as the scientists write inMolecular Psychiatry, it appears to be the most potent gene associated with human opioid sensitivity that has been identified.
A glutamate (NDMA) receptor antagonist called ketamine is looking increasingly promising as a treatment for treatment-resistant depression. Moreover, it acts within hours of injection and is already available clinically to induce and maintain general anesthesia.
But the ketamine promise doesn’t stop there. A drug company called Naurex Inc. has found that a single injection of an experimental compound similar to ketamine significantly reduced depression in subjects with treatment-resistant depression within hours, and the effect persisted for a week.
Furthermore, the drug, dubbed GLYX-13, was well tolerated, and reported side effects were mild to moderate and consistent with those observed in subjects receiving a placebo. These Phase IIa trial results were made public at the recent annual meeting of the American College of Neuropsychopharmacology.
At the American Psychiatric Association annual meeting in Toronto May 16-20, 2015, two studies were reported demonstrating the rapid efficacy of ketamine for treatment-resistant depression. In a report from Psychiatry Advisor, we learn of a study by Carlos Zarate MD of NIMH showing found that that those treated with ketamine saw improvement in depressive symptoms within two hours.
The Psychiatry Advisor article (by Jonathan Block) goes on to report two other positive studies and that a nasal spray is being developed.
“In another study — this time with an active comparator, the benzodiazepine midazolam — those who received a ketamine infusion had a rapid onset of depression improvement, based on the Montgomery-Asberg Depression Rating Scale (MADRS).
Janssen Pharmaceutica is developing esketamine, which would be administered in a nasal spray formulation for TRD. Esketamine, an enantiomer of ketamine, is in Phase II development as of July 2014.
Zarate mentioned a study that found esketamine also produced a rapid antidepressant effect, which was the same whether the drug was infused two or three times per week.
“The similarities between all the studies suggest an true biological effect is likely” with ketamine, he said. “Arguably, this is one of the first good [signs as] we have come up with a target that manipulates a specific area [of the brain] that brings about a specific effect.
[1] Psychiatric News | October 19, 2012
Volume 47 Number 20 page 16-16
see also http://archpsyc.jamanetwork.com/article.aspx?articleid=1356541
[2] Berman, R. M., et al. (2000). “Antidepressant effects of ketamine in depressed patients.” Biol Psychiatry 47(4): 351-354.
BACKGROUND: A growing body of preclinical research suggests that brain glutamate systems may be involved in the pathophysiology of major depression and the mechanism of action of antidepressants. This is the first placebo-controlled, double-blinded trial to assess the treatment effects of a single dose of an N-methyl-D-aspartate (NMDA) receptor antagonist in patients with depression. METHODS: Seven subjects with major depression completed 2 test days that involved intravenous treatment with ketamine hydrochloride (.5 mg/kg) or saline solutions under randomized, double-blind conditions. RESULTS: Subjects with depression evidenced significant improvement in depressive symptoms within 72 hours after ketamine but not placebo infusion (i.e., mean 25-item Hamilton Depression Rating Scale scores decreased by 14 +/- SD 10 points vs. 0 +/- 12 points, respectively during active and sham treatment). CONCLUSIONS: These results suggest a potential role for NMDA receptor-modulating drugs in the treatment of depression.

